September 03, 2025
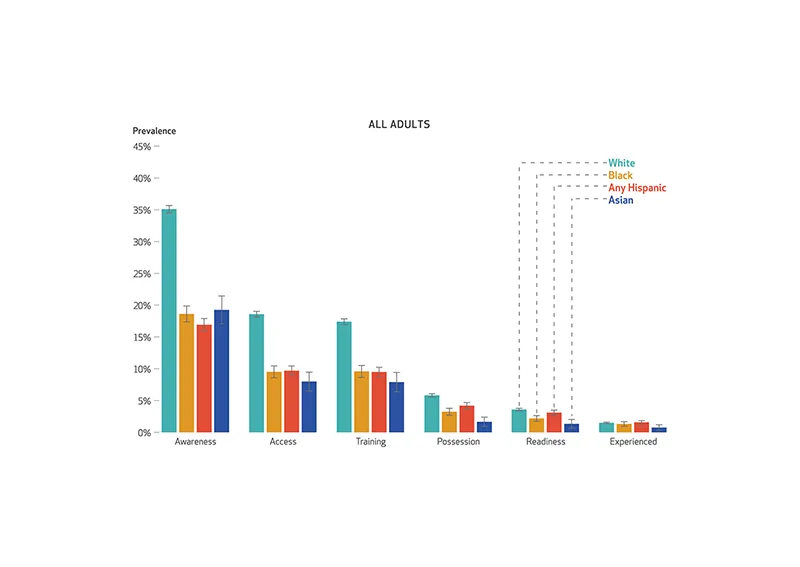
A new study published in Health Affairs reveals widening racial and ethnic disparities in naloxone engagement across the U.S., including awareness, access, possession and use. The analysis, conducted with researchers at Northwestern University, is based on data from 57,719 adults who completed the 2024 Survey of Non-Medical Use of Prescription Drugs. Researchers found that Black, Hispanic and Asian adults had significantly lower naloxone engagement compared with white adults. Naloxone is an FDA approved
medicine used to quickly reverse an opioid overdose.
The opioid epidemic has shifted in recent years, disproportionately affecting communities of color. Between 2015 and 2020, the overdose death rate for non-Hispanic Black men surged from 17.3 to 59.6 per 100,000, surpassing rates among white Americans. Hispanic populations had a 288% increase in overdose mortality between 2010 and 2020, while in 2023, American Indian
and Alaska Native people had the highest overdose death rate at 65 per 100,000.
The study also found that difference in access is a key driver of the disparities. Access is one of six stages of naloxone engagement. The other five include awareness, training, possession, readiness and experience. Gaps in any of the stages present critical public health concerns.
“The findings underscore the need for targeted, culturally responsive public health interventions,” said Joshua Black, PhD, senior statistical research scientist at Rocky Mountain Poison and Drug Safety (RMPDS).
RMPDS, a division of Denver Health, has launched innovative efforts to expand equitable access to naloxone in Colorado. One such initiative is Denver Health’s free naloxone vending machine on its hospital campus. Open to the public 24/7, the machine provides no-cost naloxone kits to anyone in need, removing barriers related to stigma, cost and accessibility.
The vending machine is part of a broader harm-reduction strategy led by Denver Health’s Center for Addiction Medicine (CAM), which offers comprehensive care for individuals with substance use disorders. CAM’s work includes clinical treatment, education and outreach designed to meet people where they are and reduce the impact of opioid-related harm.
“Our research shows racial and ethnic disparities in naloxone engagement are real and substantial,” said Lindsay Allen, lead author and assistant professor at Northwestern University. “Denver Health’s efforts — like the naloxone vending machine — are critical steps toward ensuring that lifesaving interventions are accessible to everyone, regardless of background or
circumstance.”
Researchers note that efforts such as peer-led education and investment in underserved communities will be critical to closing persistent gaps in access.
To learn more, read the Health Affairs article.

