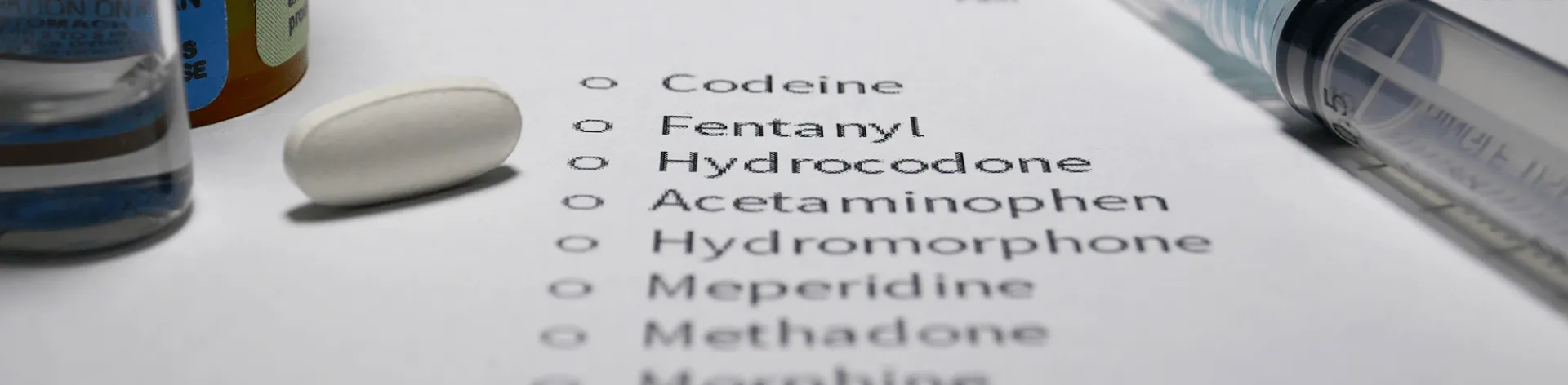
Opioid Crisis in America
The opioid addiction crisis in the United States is one of the most significant public health emergencies in this generation. Opioids are a class of drugs that include fentanyl – which the Centers for Disease Control and Prevention has classified as the most commonly used drug in overdoses, the illegal drug heroin (see how heroin hijacks the brain here) and pain relievers available legally by prescription, such as oxycodone (also known as OxyContin), hydrocodone (known as Vicodin), codeine, morphine and others.
With its hospital-wide dedication to opioid addiction eradication, supported by a full-service Behavioral Health Services and Addiction Treatment Services, Denver Health is working in partnership with the City of Denver on a five-year plan to directly confront this national health challenge.
Denver Health joins the City of Denver alongside more than 100 governmental agencies and community organizations in its Opioid Response Strategic Plan, designed to:
- Prevent Substance Abuse and Misuse
- Improve Treatment Access and Retention
- Reduce Harm
Read more on Denver Health and its partnership with the City of Denver’s strategic plan.
Opioid Addiction Help
The Center for Addiction Medicine brings together Denver Health’s robust range of opioid treatment services within a “hub-and-spoke” model that integrates resources and clinical expertise, providing a seamless, confidential and supportive journey for patients. Delivering on the “no wrong door” approach, patients who misuse opioids and present to any Denver Health clinic, medical provider or emergency facility, are rapidly connected to treatment and recovery services that best meet their needs.
Denver Health plans to expand this opioid referral model to provide patients with a broader range of treatment options for other substances such as methamphetamine.
The Center for Addiction Medicine‘s “hub” is located in Denver Health’s Behavioral Health department. The “spokes” include the Emergency Department, Psychiatric Emergency Services, methadone treatment, suboxone treatment, hospital medicine, correctional care, family health centers, Denver CARES, Denver Recovery Group, Behavioral Health Group and other community partners.
Why are Opioids so Addictive?
- Drug users often start out as occasional users. As time passes, a person goes from voluntary to compulsive drug use because, over time, addictive drugs change the brain in destructive ways.
- Drug addiction is similar to other diseases of the body, such as heart disease, because it disrupts the normal, healthy functioning of the underlying organ, has serious harmful consequences, is preventable, treatable, and if left untreated, can last a lifetime.
- Medication Assisted Treatment (MAT) does not cure opioid addiction. It treats it. Like other chronic diseases, such as diabetes, addiction is treatable and can be managed successfully.
Opioid Addiction Statistics
- From 1999 to 2016, more than 630,000 people died from a drug overdose
- In 2016, Fentanyl surpassed heroin as the deadliest drug in the United States, involved in nearly 29 percent of all overdose deaths
- In 2016, opioids were the cause of 42,249 deaths – about 66 percent of the total number of drug overdose deaths
- In 2016, the number of overdose deaths involving opioids (including prescription opioids and illegal opioids like heroin and illicitly manufactured fentanyl) was five times higher than in 1999
- On average, 115 Americans die every day from an opioid overdose
- The 2017 Colorado drug overdose death total was 1,012
Additional Opioid Addiction Information and Resources
The opioid epidemic requires Denver Health to envision a different care practice. We provide help for recovering addicts, including 24/7-access to treatment for opioid detoxification and treatment of withdrawal symptoms for all substances in our emergency department. We are expanding access to Medication Assisted Treatment (MAT), working to transform treatment into an on-demand service including biological, psychological and social evaluations, known as the Center for Addiction Medicine at Denver Health.
Our Goal
Improve treatment access and retention
Strategy
Increase participation/enrollment of people with substance use disorders in treatment services
Activity
Establish a regional intake induction center for rapid treatment admissions
As part of a strategic growth initiative in 2018, Denver Health is committed to establishing a Center for Addiction Medicine. The Center will offer care to provide patient access to an array of substance treatment services. Services include prevention and education, harm reduction, formal treatment and management of addiction disorders, along with post‐treatment services, tools and resources that support ongoing recovery.
Expected Outcomes
- Create 24/7-access to Medication Assisted Treatment (MAT) on demand
- Develop a standardized evaluation/transfer packet and referral system
- Increase capacity across the opioid treatment program system
- Increase the volume of drug offenses to diversion
- Assess community need for 24/7 access to MAT on demand
In an era of increasing opioid addiction, Denver Health advances opioid treatment through our integrated opioid service delivery model, Colorado’s first Opioid Treatment Hub and Spoke.
Results
- Expand capacity
- Reduce costs
- Reduce re-admission
- Improve health outcomes
Hub and Spoke Method
 The Hub and Spoke method focuses on narcotic treatment programs as comprehensive treatment hubs. The Hub, provides comprehensive addiction and mental health services, is designed to stabilize persons who are opioid addicted and relies on the spokes, which are community medical practices to accept transfer of stabilized, less clinically complex, patients into their clinics to maintain opioid use disorder treatment.
The Hub and Spoke method focuses on narcotic treatment programs as comprehensive treatment hubs. The Hub, provides comprehensive addiction and mental health services, is designed to stabilize persons who are opioid addicted and relies on the spokes, which are community medical practices to accept transfer of stabilized, less clinically complex, patients into their clinics to maintain opioid use disorder treatment.
- Due to the relapsing nature of addiction, it is imperative to maintain coordination between the Hub and Spoke as patients are likely to transfer between high, moderate and low levels of care throughout their recovery Journey. To protect the health care resources of the Spoke, the Hub is committed to re-admit an opioid use disorder patient at the request of the Spoke team.
- Successful Hub and Spoke service integration provides a highly coordinated level of care for patients. This care model better addresses treating a patient’s multiple needs, including co-occurring medical and mental health diagnoses. By optimizing a comprehensive system of care, the greatest benefit to public health can be achieved.
Community Partnership
By integrating Medication Assisted Treatment (MAT) models across Denver Health’s broad framework, including the Department of Psychiatry, Ambulatory Care Clinics, Inpatient and Emergency medicine units, along with Denver Public Health’s ability to conduct research and education to reduce the negative impacts of opioid abuse; Denver Health has become Colorado’s opioid addiction treatment pioneer. Denver Health’s clinical capabilities, current cross-systems initiatives have the ability to deliver a significant expansion of opioid treatment leading us to be Colorado’s first:
- Hub & Spoke
- Emergency Department to induct buprenorphine (Suboxone) with next day access to MAT continuation
- First inpatient hospital to provide methadone to maintain opioid tolerance and reduce fatal overdose risk post-hospitalization
- First narcotic treatment program to expand to seven-day access
- First narcotic treatment program to provide 100 percent of our patients with NARCAN, an FDA-approved nasal spray for the emergency treatment of a known or suspected opioid overdose
Our model guarantees a strong community response to opioid addiction through our cross-system integration. We collaborate to design integrated programming that reflects the chronic and relapsing nature of addiction. We establish a smooth, efficient, and reliable means of engaging patients into treatment, and transfer patients between physical and behavioral health care to ensure they are stabilized and successfully treated by a designated provider in their home community.
Preventing Opioid Use Before it Starts
- Specific youth behavioral health issues are identified and collective awareness of how to address them is raised
- Long-term prevention of youth behavioral health issues
- A greater number of youth identify using positive coping mechanisms for stress
Methadone
A synthetic opioid prescribed to treat opioid addiction. Methadone can only be provided by a licensed narcotic treatment program; commonly referred to as a ‘methadone clinic.’
Buprenorphine (Commonly known under the brand-name Suboxone)
Buprenorphine is a narcotic medication used to treat opioid addiction. It is commonly known under the brand-name Suboxone. Buprenorphine can be provided by a physician with special training or within a narcotic treatment program.
Benefits of Methadone and Buprenorphine (Suboxone)
Methadone and Buprenorphine (Suboxone) stop the effects of withdrawal, decrease the cravings for opioids, block the effects of opioid misuse and reduce relapse. Unlike heroin and short-acting opioids, the effects of methadone and buprenorphine last 24 hours, so patients only need to take it once a day. Both drugs provide a steady state of medication and do not cause heroin’s physiologic disturbances.
Naltrexone (Commonly known under the brand-name Vivitrol)
Extended-release injectable naltrexone is another medication tool that treats opioid addiction. It is commonly known under the brand-name Vivitrol. Injectable Naltrexone can be provided by any healthcare provider who is licensed to prescribe medications. The medication can also be provided within a narcotic treatment program. Naltrexone binds to and effectively blocks opioid receptors. It prevents receptors from responding to opioids and is reported to reduce opioid cravings.
Denver Health's expert care teams include physicians, psychiatrists, nurses, clinical psychologists, social workers, professional counselors and case managers. Outpatient Behavioral Health Services offers professional, multi-disciplinary substance and mental health treatment through a number of specialized clinical care teams. Substance treatment includes Medication Assisted Treatment (MAT) (methadone and buprenorphine (Suboxone)) through a licensed narcotic treatment program (methadone clinic) plus buprenorphine and depo-naltrexone through office-based opioid treatment. Denver Health provides patients on MAT with care that includes intensive outpatient and transitional residential treatment. The system also includes specialized services for women with dependent children, addiction services for pregnant women, co-occurring psychiatric support and access to MAT within primary care.
Methadone Clinic
A methadone clinic (Narcotic Treatment Program) is a clinic which has been established for the dispensing of methadone for the sole purpose of opioid addiction. Patients are asked to attend the clinic for medication and therapy services. Medication is dispensed daily until patients stabilize and earn take-home medication. The patient earns take-home medication after their random urine drug tests show no illicit substances or alcohol in their system, time in treatment and improvement in psycho-social symptoms. For patients who do not wish to discontinue the use of an illicit substance, you are still welcome in this clinic setting, but you will need to come every day for your medication. Anyone 18-years-old and older, who has been addicted to opioids for 12 months or more, can come to the clinic and seek methadone treatment.
Denver Health’s methadone clinic provides both methadone and buprenorphine (Suboxone).
Buprenorphine (Suboxone) Clinic
Buprenorphine (Suboxone) can be provided in an outpatient clinical setting. Such clinics are referred to as Office-based Opioid Treatment (OBOT). OBOTs have been established to provide Medication Assisted Therapy in a non-methadone setting. In OBOT, patients will receive a prescription from a physician. To continue to receive buprenorphine from the OBOT you will have to be abstinent from all substances of abuse including alcohol and benzodiazepines. Anyone 18-years-old and older who is addicted to opioids can come to the clinic and seek buprenorphine treatment.
In 2020, Denver Health’s OBOT will relocate to the new Outpatient Medical Center.
Colorado's First Medication Assisted Therapy (MAT) On-Demand
Having a hard time getting into Medication Assisted Treatment (MAT)? Medical staff and clinical social workers are prepared to begin MAT services and treatment referral planning at Denver Health’s Emergency Department 24-hours-a-day, 7-days-a-week. All patients being inducted into MAT by Denver Health physicians, will engage in physical, psychological and social evaluation of substance use and mental health disorders. Triage planning efforts will begin onsite during MAT initiation and will focus on the interventions and activities needed to prepare the patient for access to their home opioid treatment program while targeting accessibility based on patient preference and behavioral health needs. Colorado’s first MAT on-demand program is led by Denver Health and receives city funding in partnership with the City and County of Denver’s opioid treatment programs. The program will focus on Denver adults with a DSM-V Opioid Use Disorder (OUD) (female and male), 18-years-old and older. The MAT Induction Transfer Center (MAT-ITC) population of focus will encompass adult individuals of all races and ethnicities, sexual orientations, veterans and those with and without other mental or physical disabilities and pregnant women.
Substance Use Treatment Line
We offer substance use screening, referrals, information related to Suboxone/Methadone and non-OUD treatment options. For screening or information, call 303-436-5711.
Substance Treatment Phone Line
303-436-5711, calls are answered Monday-Friday, 9 a.m. - 5 p.m. (excluding holidays)
This line is staffed by experienced substance treatment experts who can provide brief screening, recommendations, and guidance to individuals, friends/families, and other professionals on accessing substance treatment both here at Denver Health, and through other programs in our Denver community and surrounding areas.
Other Resources
Denver Health is state licensed and joint commissions accredited in the treatment of substance abuse and behavioral health. The Substance Abuse and Mental Health Services Administration encourages patients to choose a treatment location that is effective in treatment and recovery from substance use disorders based on these five signs of quality treatment, which Denver Health meets or exceeds:
- Accreditation: Licensed or certified by the state, currently in good standing, qualified, properly trained and licensed staff.
- Medication: FDA approved medication for recovery from alcohol and opioid use disorders. There are no FDA approved medications to help to prevent relapse from other problem substances.
- Evidence-Based Practices: Treatments that have been proven to be effective in treating substance use disorders including medication management therapies, motivational therapy, cognitive behavioral therapy, drug and alcohol counseling, education about the risks of drug and alcohol use and peer support and help to obtain medical care for physical health issues.
- Families: Family members are included in the treatment process because family members have an important role in understanding the impact of addiction on families and providing support.
- Supports: Ongoing treatment and supports beyond just treating the substance issues. For many people addiction is a chronic condition and requires ongoing medication and supports. Quality programs provide treatment for the long term which may include ongoing counseling or recovery coaching and support, and help in meeting other basic needs like sober housing, employment supports and continued family involvement.
Denver Health serves all persons seeking health care for a substance use disorder. Our patients come from all walks of life and communities beyond the city and county of Denver. If we’re not the best suited clinic, or we’re not an in-network provider, we will help navigate patients to another service provider. As stated in our mission, we will always care for all.
Watch this short video about the recovery of one of our former methadone clinic patients, Christy Polito.
Deadly heroin and prescription opioid overdoses are rising and associated health, economic, social and legal impacts are threatening to skyrocket. This requires Denver Health to envision a different care practice, one that fundamentally, not incrementally, changes our traditional model of medication assisted treatment delivery.
Denver Health, with support of community partnerships, offers a framework of integrated care with a community response to opioid addiction through cross-system integration. We plan to collaborate in a meaningful way to design integrated programming that reflects the chronic and relapsing nature of addiction; establish a smooth, efficient, and reliable means of engaging persons into treatment; and transfer patients between physical and behavioral health care to ensure they are stabilized and successfully treated by a designated provider in their home community.
Our clinical capabilities are in place; at Denver Health we do this because we care about our community members. Watch Behavioral Health Services clinical support specialist John Mills talk about how his work at Denver Health is personal to him.